Synthetic Male Sling
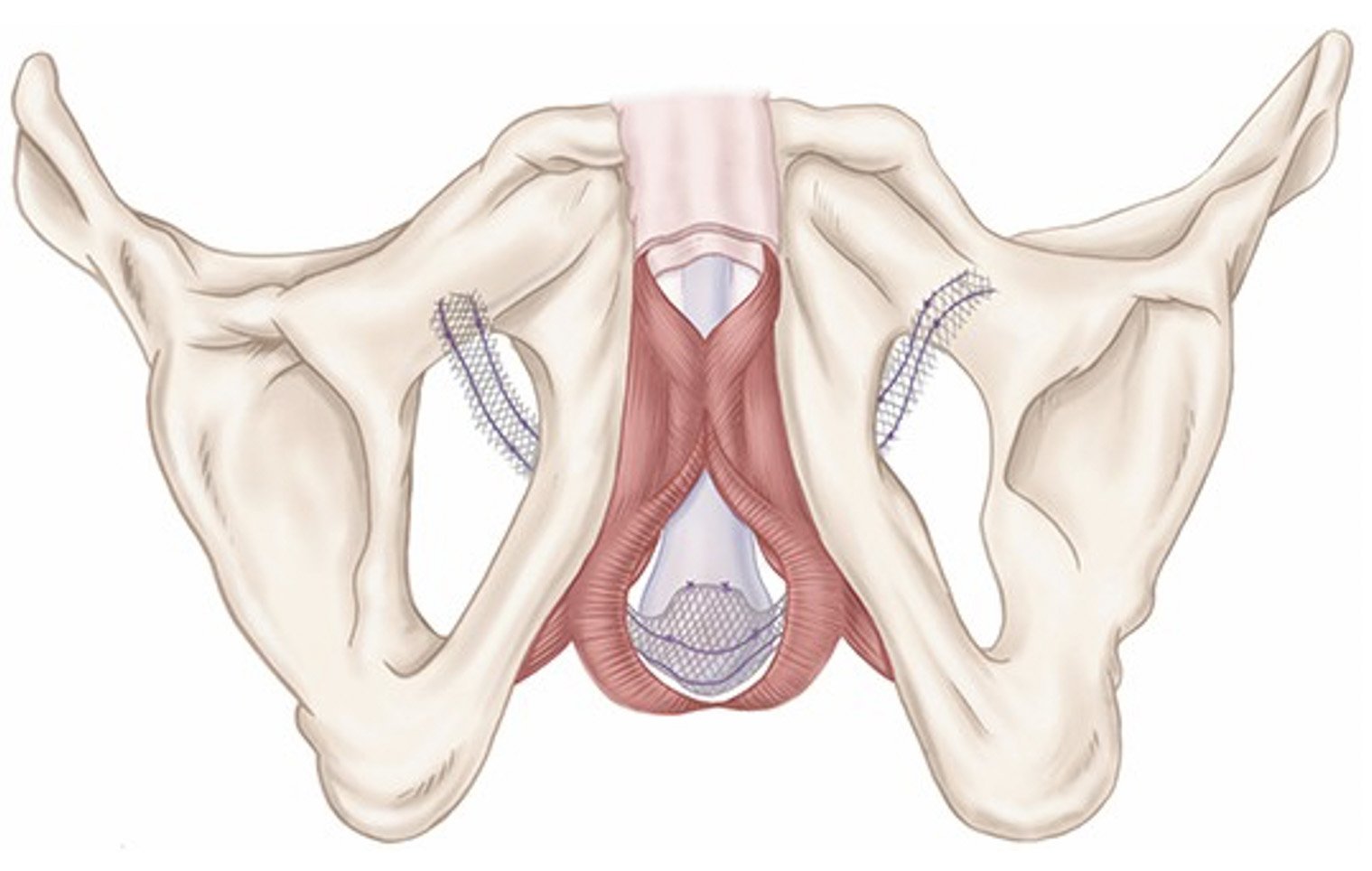
Figure 1 – Positioning of synthetic male sling.
What are the indications for insertion of synthetic male sling?
An artificial urinary sphincter (synthetic male sling) is an effective treatment for men with mild stress urinary incontinence (involuntary leakage). In the vast majority of men, this is done for post-prostatectomy urinary leakage. It is not an effective treatment in men with previous pelvic radiation.
What pre-operative work up is needed before the procedure?
Your urologist will organise any necessary urine and blood tests at your consultation prior to your procedure. You will have a cystoscopy to rule out any blockages in your waterpipe and you may need urodynamic studies if there is any doubt about the diagnosis.
It is important that any urine and skin infections around the genital areas are completely treated. If you have diabetes, your urologist will liaise with your GP / specialist to ensure it is well controlled to reduce risk of infection after the operation. You MUST stop smoking before your prosthesis surgery.
You will be given an antibiotic wash, which you should use to clean your abdomen and genital area for 3 days before the operation. You should not shave or clip any hair in your genital area – this will be done by the urologist at the time of surgery.
If you take any blood thinning medication such as aspirin, warfarin, plavix (clopidogrel) and anticoagulants, you should discuss this with your urologist, as they may need to be stopped temporarily.
Please ensure you return any admission forms given to you to be filled out back to the hospital.
What happens on the day of the procedure?
You will be admitted on the morning of your procedure and given intravenous antibiotics early in the morning of surgery. You will be given fasting instructions prior to your admission (usually for 6 hours prior to the procedure). You should bring a list of your medications with you to the hospital. After you are admitted, your urologist will see you in the morning to discuss the surgery. An anaesthetist will see you to discuss the general anaesthetic before you are taken to the operation theatre. You may be provided with a pair of TED stockings to wear to prevent blood clots from developing and passing into your lungs.
What does the procedure involve?
A synthetic sling (made from plastic mesh) is placed under your urethra (waterpipe), near to where the prostate gland used to be. It reduces leakage by providing support to the urethra. Satisfaction rates are approximately 70-80%.
After a general anaesthetic, you are given some intravenous antibiotics to reduce the chance of infection. The genital area is shaven and cleaned with antiseptic for five to 10 minutes to minimise the risk of infection. A small cut is made in the skin between your scrotum and back passage to place the sling around the urethra. A small stab incision is made near the groin on both sides to position and tighten the sling appropriately. You will have a catheter to drain urine from your bladder overnight. The wounds are closed with dissolvable sutures. A waterproof dressing is used to cover the wounds. The procedure takes approximately 1 hour to perform.
You will stay in hospital overnight for more intravenous antibiotics the next morning. Your drain and catheter will be removed the next morning and you will be discharged with the dressing intact and on oral antibiotics for 1 week.
Are there any risks or side‑effects of insertion of synthetic male sling?
Swelling and bruising of the area lasting a few days 80-100%
Minor ooze of the wound 10-20%
Minor infection of the incision requiring antibiotics 5-10%
Infection / bleeding needing removal of sling 3-5%
New onset of urgency and urge-related leakage 5-10%
Failure to produce significant improvement in stress incontinence 5-10%
Temporary inability to pass urine needing catheter placement 3-5%
Persistence tenderness at the surgical site or groin pain 2-3%
Erosion / Mesh problems relating to the sling 2-3%
Injury to bladder, urethra or other organs during implantation 1-2%
Major cardiovascular or anaesthetic problems - rare
Important note regarding mesh sling surgery
There is currently a restriction for vaginal mesh surgery in women although it’s position currently does not apply to men. Whilst these problems have not being encountered in men undergoing mesh surgery, long-term outcome data for the use of mesh in men is lacking. Your urologist will discuss this with you. If removal of mesh in men becomes necessary, it is a complex procedure, which may not be technically possible.
What should I expect on discharge when I get home?
You will experience some swelling, discomfort and sensitivity at the operative site for a couple of weeks, which should settle with time and with paracetamol and/or ibuprofen. Take your antibiotics as prescribed for a week. Keep the waterproof dressing on for 7 days. The skin sutures are self-dissolving (takes 2-4 weeks) and do not need to be removed.
After 5-7 days, you can begin light activities again and desk work. You should only return to strenuous activity and driving after 4 weeks, and when you are completely pain free and your GP is happy with your progress. You should refrain from sexual activity for a minimum of four weeks.
If you develop swelling, fevers or significant pain and redness at the site or if you are having trouble passing urine, you should contact your GP or urologist.
What follow-up will I need?
You should see your GP in 1-2 weeks for a wound check. Your urologist will see you in the clinic in 6 weeks.